Telehealth vs. In-Person Medical Marijuana Consultations
Written By QuickMedCards. Updated February 5, 2026
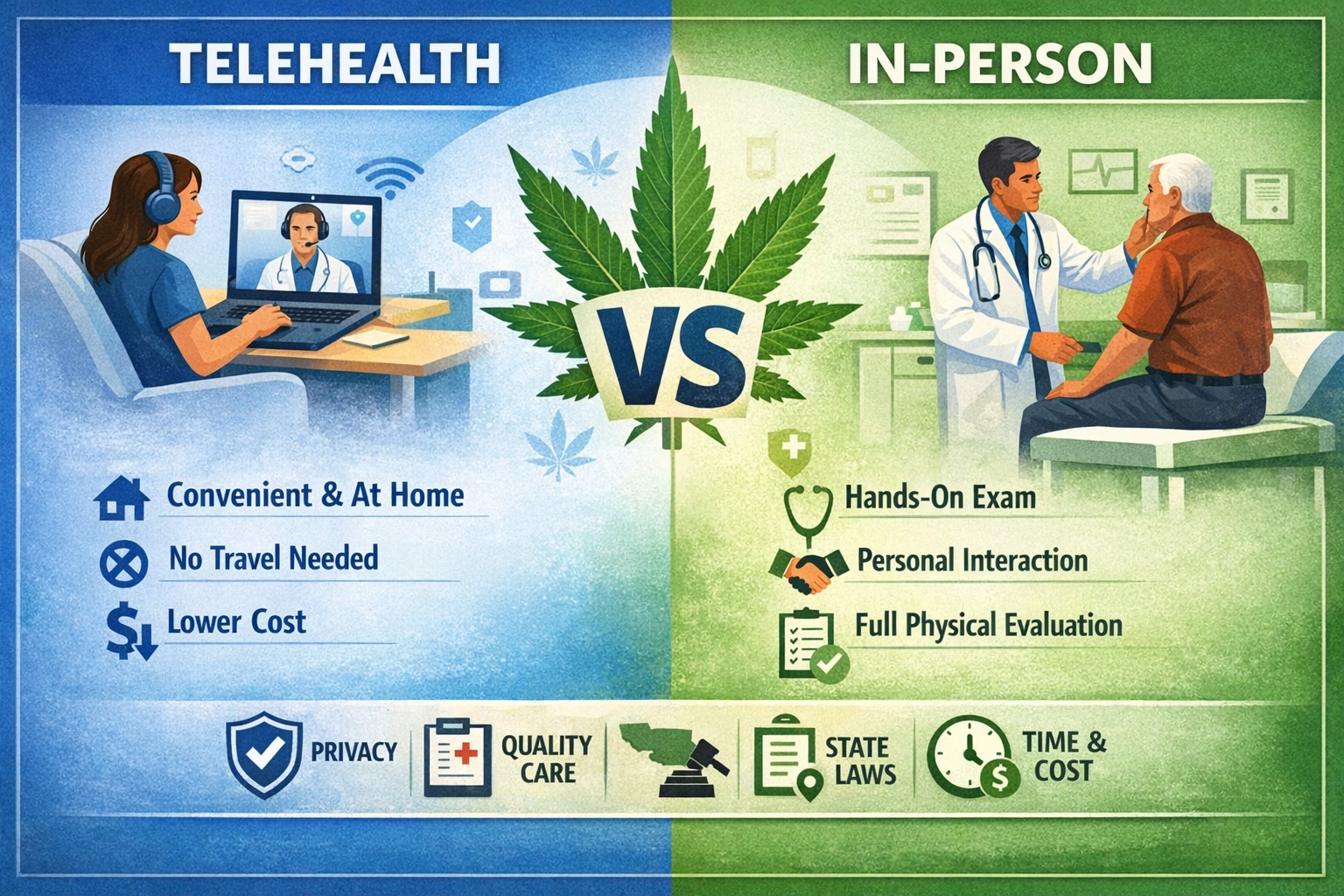
You need a medical cannabis card. You have two options: a video call or a visit to the doctor’s office.
Some states strictly require in-person consultations in specific cases. Most states accept both.
The experience between the two isn’t the same. Cannabis telemedicine offers convenience. In-person visits offer something else entirely.
When you compare online vs in-person medical cannabis evaluation services, the differences go beyond just location. They impact your costs, privacy, and the time it takes to get certified. One might save you time. The other might give you more thorough care.
Which approach fits your situation? Let’s look at what each one actually offers.
By the end of this page, you will have the answers to these questions:
- What do medical marijuana evaluations involve?
- How do telehealth and in-person consultations compare for privacy, quality, and follow-up care?
- What state rules commonly affect whether telehealth is allowed for first-time patients?
- What is a patient-provider relationship?
- How do states handle telehealth for medical marijuana?
- What to expect from telehealth and in-person consultations, and which option is right for you?
- How can you choose a reputable provider and avoid “card mill” red flags?
- What should you prepare so your appointment goes smoothly?
Looking for a Medical Marijuana Doctor?
What Do Medical Marijuana Evaluations Involve?
A proper medical marijuana evaluation is not a quick yes or no decision. Whether the visit happens in-person or through telehealth, the clinician’s role stays the same. They assess your symptoms, review your history, and determine whether medical cannabis may be appropriate for you. Just as important, they explain potential risks and document the visit to meet state program rules.
These visits also differ from standard doctor appointments in one key way. In most states, clinicians issue a certification or recommendation, not a traditional prescription. That distinction exists because medical cannabis programs operate outside the normal pharmacy system, even though the clinical standards still apply.
A thorough marijuana evaluation commonly includes:
- Review of symptoms and health history
- Discussion of past treatments and what has or has not helped
- Medication review to identify possible interaction risks
- Safety screening for pregnancy, heart conditions, mental health history, and substance use
- Education on potential side effects and safer use basics
- Follow-up planning, especially for first-time medical cannabis patients
At its core, a medical marijuana evaluation is about informed care, not convenience alone. The format may change, but the responsibility to deliver a complete, compliant, and patient-focused consultation does not.
Telehealth vs. In-Person Medical Marijuana Consultations
Telehealth is no longer a novelty in health care. It became a necessity during COVID. Since then, it has settled into something more permanent. For many patients, it is now a normal way to see a clinician, not a backup option.
This shift matters for medical marijuana consultations. Cannabis telemedicine allows patients to complete evaluations remotely using secure video technology. It falls under the broader umbrella of telehealth, which covers many types of digital health services. Telemedicine is the clinical piece of that system. It focuses on diagnosis, evaluation, and treatment between a doctor and a patient who are not in the same place.
At the same time, in-person consultations remain the traditional model of care. They’ve been the foundation of medicine for centuries. Face-to-face visits still offer advantages that cameras can’t replicate. Some patients prefer them. Some conditions require them. Some states mandate them.
The question isn’t which method is “better” overall. It’s which one fits your specific situation. Each approach has distinct strengths and trade-offs across convenience, cost, privacy, quality, and access.
Let’s break down how they actually compare.
Convenience
Marijuana telemedicine wins on logistics. You join a video call from your couch. No commute. No waiting room. No juggling childcare or burning half a day off work.
For some patients, that convenience is more than a perk. It’s the difference between getting care and going without. If you have mobility issues, a chronic pain flare-up, or live an hour from the nearest clinic, telehealth removes real barriers.
In-person visits require more planning. You drive to the office. You sit in the waiting room. You factor in traffic and parking. The appointment itself might take fifteen minutes, but the total time commitment is often two hours or more.
Convenience alone should never define quality. Telehealth works best when it delivers the same level of care without cutting corners. When done right, convenience supports access without sacrificing the integrity of the evaluation.
Greater Accessibility
Telehealth opens doors that geography used to keep closed. If you live in a rural area with no nearby cannabis clinic, you can now connect with a cannabis doctor miles away. No multi-hour drive. No hotel stay. Just a video call.
Access to specialists improves, too. Some states have only a handful of certified cannabis physicians. Telehealth lets you consult with experts who would otherwise be out of reach. For patients dealing with complex conditions or rare symptoms, that expanded network matters.
The data backs this up. A 2017 study found that telemedicine helped urban patients treat acute illnesses while cutting costs by reducing emergency room visits. Doctors reported that most standard appointments could be handled remotely. The technology broke down real barriers to care.
But telehealth isn’t universally accessible. It requires reliable internet, a private space to talk, and basic comfort with technology. Some patients don’t have those things. Others prefer face-to-face interaction or need help with paperwork on-site.
In-person visits still serve people who lack digital access or simply work better in a physical setting. A clinic staff member can walk you through forms. You also don’t need to worry about your connection dropping mid-appointment.
Accessibility isn’t one-size-fits-all. Telehealth expands reach for most patients, but in-person visits remain more accessible for some.
Evaluation Quality and “Standard of Care”
A telehealth evaluation should meet the same clinical standards as an in-person visit. The Federation of State Medical Boards confirms that doctors can establish a legitimate physician-patient relationship through telemedicine without ever meeting face-to-face. The requirement is simple: meet the standard of care.
In practice, the two formats have real differences. In-person visits allow hands-on physical exams when needed. A doctor can check your blood pressure, listen to your heart, or examine a painful joint. Telehealth has limits here, though certain exam elements still work remotely. A clinician can observe your movement, breathing patterns, or visible skin conditions through video.
The Department of Health and Human Services acknowledges these constraints. Telemedicine documentation should reflect what the doctor observed and what couldn’t be performed due to equipment limitations. That transparency matters.
Quality depends more on the clinician than the medium. A reputable telehealth provider asks detailed questions, not just checkbox prompts. They confirm your identity and location. They review relevant medical records when appropriate. They explain risks, benefits, and alternatives. They document everything like any proper medical appointment.
Red flags look the same online or in person. If the process feels like “fill out a form, get instant approval,” that’s not healthcare. That’s a rubber-stamp operation, cutting corners.
The format doesn’t determine quality. The clinician’s rigor does.
Privacy and Security
Privacy has become a front-and-center issue in medical care. That is especially true for cannabis patients.
Telehealth visits rely on digital platforms that handle protected health information. When the provider is a covered health care entity, HIPAA rules still apply. Federal guidance makes it clear that telehealth does not lower privacy standards. It simply changes the setting where care takes place.
At Quick Med Cards, appointments are HIPAA-compliant and conducted through Doxy. Conversations with your doctor stay private and follow strict medical privacy requirements.
That said, privacy during a telehealth visit also depends on the patient’s environment. Taking the call in a private space, using headphones, avoiding public Wi-Fi, and understanding what platform is being used all help reduce risk. These small steps go a long way in keeping sensitive conversations secure.
In-person visits have their own privacy considerations. Some patients feel more at ease speaking face-to-face in a closed exam room. Others prefer telehealth because it avoids being seen entering a cannabis related clinic. Both concerns are valid and deeply personal.
Privacy and security are not about choosing the “right” format. They are about choosing the setting that makes you feel safest sharing your health information.
Enhanced Follow-Up Care
Follow-up care has changed in meaningful ways. Telehealth has made staying connected much easier after the initial evaluation.
Once a clinician understands your condition, virtual check-ins tend to work well. Telehealth allows patients to discuss symptom changes, side effects, or product tolerance without repeating the full effort of an office visit. Many states also allow telehealth for renewals after an initial in-person exam, which reduces friction while keeping care compliant.
In-person follow-ups can still be useful, especially when a physical exam is needed. But for routine monitoring, travel and scheduling often slow things down. Telehealth removes those barriers, making it easier to check in sooner rather than later.
This flexibility supports better long-term care. Patients are more likely to attend follow-ups when they are simple to schedule. Clinicians can monitor progress more consistently and adjust guidance as needed. Over time, that regular contact leads to more personalized and better managed care.
Enhanced follow-up is not about replacing in-person visits. It is about making ongoing care easier to access and easier to maintain.
Reduced No-Show Rates
Missed appointments disrupt care. Telehealth has helped change that pattern.
Virtual visits make it easier for patients to show up. There is no commute to plan around. No last-minute transportation issues. No added time off work. When appointments fit more naturally into daily life, patients are more likely to attend them.
In-person visits face more obstacles. Travel delays, schedule conflicts, and symptom flare-ups can all lead to cancellations or no-shows. Even motivated patients can struggle to make it to a physical office consistently.
Evidence supports the shift. A 2024 systematic review found that patients using telehealth services were significantly less likely to miss appointments compared to those receiving in-person care. Fewer no-shows helped maintain treatment plans and supported better continuity of care.
Reduced no-show rates are not just a scheduling win. They reflect better access, stronger engagement, and more reliable follow-through.
Cost Effectiveness
Cost has become a bigger part of health care decisions. Telehealth has shifted that equation.
Telemedicine reduces many of the hidden expenses tied to in-person visits. There is no travel cost. Less time off work. Fewer childcare or transportation expenses. In many cases, the appointment itself also costs less.
In-person consultations often come with higher indirect costs. Even when the visit fee is similar, travel time and missed work can make the total price higher than expected. For patients managing chronic conditions, those costs add up quickly.
This is where providers matter. Quick Med Cards is often the cheapest option for getting a medical marijuana card. And when it is not, the price beat guarantee matches competitor pricing, so patients do not overpay for care. That pricing flexibility removes cost as a barrier while keeping the evaluation legitimate.
Public health research supports this shift. A CDC research anthology found that telemedicine lowers costs by reducing hospital admissions and unnecessary emergency visits. By streamlining care, telehealth delivers financial relief without sacrificing quality.
Cost effectiveness is not about cutting corners. It is about delivering the same standard of care in a way that saves patients time and money.
Infection Risk Reduction
Infection risk became impossible to ignore in modern health care. Telehealth changed how patients think about exposure.
Remote consultations remove the shared spaces that increase the risk of infection. There are no waiting rooms. No crowded clinics. Patients attend their appointment from home, which limits contact with others who may be sick. This became especially important during COVID, when minimizing exposure was a public health priority.
In-person visits still carry unavoidable exposure. Even well-managed clinics involve shared surfaces and close contact. For many patients, especially those with weakened immune systems, for example, patients with HIV/AIDS or chronic conditions, that risk is not trivial.
Infection risk reduction is a practical advantage of telehealth. It allows patients to receive care without adding unnecessary health concerns.
How Do the Rules Vary by State?
State rules are where most of the confusion begins. Medical marijuana programs are run at the state level, not federally. That means telehealth and in-person requirements can look very different depending on where you live.
Two realities apply almost everywhere. Your physical location during the visit matters, and the clinician must be authorized to practice in that state. Even when telehealth is broadly allowed, medical marijuana programs often add extra certification rules on top of general telemedicine laws.
Because of this, legitimate providers follow strict verification steps. They confirm your identity, your current location at the time of the visit, and their own authorization to evaluate patients in your state. These checks are required for the certification to be valid.
For patients, the easiest way to get clarity is to review their state-specific rules ahead of time. Our state cannabis laws page provides a clear starting point for understanding whether telehealth is allowed and what your program requires. If a clinic claims it can evaluate anyone, anywhere, without verifying details, that is a clear warning sign.
What Is a Patient-Provider Relationship?
A valid certification starts with a real patient-provider relationship. This requirement exists to make sure medical marijuana care is legitimate, accountable, and ongoing.
In cannabis telemedicine, the relationship is not just a formality. Many state medical marijuana programs require that a medical marijuana doctor online establish the same clinical responsibility as they would in person. That means the provider is responsible for your care, not just the approval.
States tend to define this relationship in similar ways. Using Hawaii as an example, a bona fide patient-provider relationship is established when the clinician does the following:
- Completes a full assessment of your medical history and current condition
- Reviews relevant medical records when medically appropriate
- Provides follow-up care and ongoing evaluation during cannabis use
- Monitors how medical cannabis is affecting your symptoms
- Maintains medical records that meet accepted clinical standards
This structure exists for a reason. It ensures that evaluations are thoughtful, follow-ups are available, and records meet accepted medical standards. A true patient-provider relationship is what separates real medical care from one-time approvals that do not meet program requirements.
Real-World Examples of How States Handle Telehealth for Medical Marijuana
Some states allow a medical marijuana doctor to evaluate first-time patients. Others only permit telehealth for renewals.
These differences matter. Below, we look at states that allow telemedicine for first-time evaluations and those that restrict online visits to returning patients only.
States That Allow Telemedicine for First-Time Patients
A growing group of states now allows first-time patients to complete their marijuana evaluation online with a licensed medical cannabis doctor. For example:
- Arizona
- Connecticut
- Delaware
- Georgia
- Hawaii
- Illinois
- Iowa
- Louisiana
- Maine
- Maryland
- Minnesota
- Michigan
- Missouri
- Montana
- New Jersey
- New Mexico
- New York
- North Dakota
- Ohio
- Oklahoma
- Pennsylvania
- Texas
- Virginia
- West Virginia
Hawaii shows how this shift has played out in practice. First-time patients were once required to see a cannabis doctor in person. That requirement ended on September 18, 2025, when Act 241 took effect. Since then, both initial certifications and renewals can be completed through telehealth.
The message from these states is clear. Telemedicine is now accepted as a legitimate starting point for medical marijuana care, not just a follow-up option.
States That Allow Telemedicine for Renewals Only
Some states have taken a more cautious approach. They still require first-time patients to be evaluated in person, but they allow telehealth once a patient is already established in the program.
In these states, the first visit must happen face-to-face. After that, renewals can often be completed remotely. This model keeps the initial exam traditional while adding flexibility later.
The states that follow this approach include:
At Quick Med Cards, this distinction matters. In Arkansas, our doctors can help patients who are renewing their medical marijuana certification through telehealth. Patients do not need to return to their original certifying doctor. However, our doctors cannot certify first-time Arkansas patients online. The same rule applies in Kentucky, where telehealth is limited to renewals only.
These states show a clear middle ground. Telemedicine is accepted for ongoing care, but in-person visits remain the starting point.
What to Expect in a Telehealth Consultation
A cannabis telemedicine consultation usually takes place over secure video. In some cases, audio-only visits are allowed. When the provider is a covered health care entity, HIPAA privacy rules still apply. The visit follows a clinical flow, just without the exam room.
A typical telehealth consultation usually includes the following:
- Identity verification, such as confirming your name, date of birth, and sometimes a photo ID
- Review of your medical history, symptoms, past treatments, and daily impact
- Medication and safety screening, including mental health history, pregnancy status, and substance use risks
- Education on benefits, side effects, product types, and safer dosing basics
- Clear next steps if you qualify, including state registry instructions when required
When done properly, a telehealth visit feels organized and thorough. You finish the appointment knowing where you stand, what comes next, and how to move forward with confidence.
What to Expect in an In-Person Consultation
In-person consultations follow the traditional model of care. For many patients, that familiarity still matters.
The core of the visit is similar to telehealth. You review your symptoms, medical history, and past treatments with a clinician. The difference is the setting and the tools available. In-person visits allow for vitals to be taken, brief physical exams, and direct observation that can be harder to capture on video.
This format often works well for patients with more complex medical histories or those who want a hands-on exam. It can also help patients who need guidance with paperwork or state registration steps, since support is available on-site.
Privacy plays a role, too. Some patients feel more comfortable discussing sensitive symptoms in a private exam room rather than at home. For them, the in-person setting adds a sense of security and focus.
An in-person consultation offers depth, structure, and reassurance. It remains a strong option for patients who value face-to-face care and a traditional clinical experience.
How to Decide Which Option Fits You Best
Choosing between telehealth and in-person care comes down to fit, not right or wrong. The best option depends on your comfort level, your health needs, and what your state allows.
Telehealth Is Often a Strong Fit When
Telehealth works best when access and flexibility matter most. It removes barriers that make care harder than it needs to be.
Telehealth is often a strong fit when:
- You have transportation barriers, mobility limits, or a packed schedule.
- You live far from a participating clinic.
- Your symptoms make travel difficult, such as chronic pain flare-ups.
- You want easier follow-up care after the initial visit.
- Your state allows telehealth for your situation.
When these conditions apply, telehealth removes friction and makes care easier to access without lowering the standard of the evaluation.
In-Person Is Often a Better Fit When
In-person care remains important for many patients. It offers structure, hands-on assessment, and direct interaction.
In-person consultations are often a better fit when:
- Your state requires an in-person exam for first-time certification.
- You have a complicated medical history or multiple interacting conditions.
- You want a hands-on physical exam or have concerns about side effects.
- You do not have reliable internet or a private place for a video visit.
- You feel more comfortable building trust face-to-face.
When these factors apply, an in-person visit provides clarity and confidence that can be harder to achieve remotely.
How to Choose a Reputable Medical Marijuana Provider
The format of the visit matters less than who is providing the care. A good clinician makes the difference, whether the appointment is online or in person.
A reputable online medical marijuana card service follows state rules and medical standards. The cannabis doctor should be licensed and authorized to evaluate patients in your state when required. For example, Oklahoma reminds patients that doctors must be registered with the state medical marijuana program (OMMA) to recommend cannabis legally and encourages patients to verify that registration. Legitimate providers are transparent about these requirements and explain why they matter.
There are also clear warning signs to watch for. Be cautious if you see:
- Claims that everyone qualifies
- No medical history questions
- No identity verification
- No discussion of side effects, interactions, or safety concerns
- Pressure to buy products from a specific dispensary
Choosing the right provider protects both your health and your certification. When the evaluation is thorough, compliant, and patient-focused, you can move forward with confidence.
Preparing for Your Appointment
Before your appointment, it helps to have a few things ready. This keeps the visit focused on care, not paperwork.
Have these items available:
- A current photo ID and proof of residency if your state requires it
- A short list of diagnoses and symptoms, including when they started and how they affect daily life
- A complete list of current medications and supplements
- Relevant medical records, when available, especially for first-time certifications
It also helps to come prepared with questions. Writing them down keeps the conversation clear and productive.
Common questions patients ask include:
- What side effects to watch for based on personal health history
- How cannabis may interact with current medications
- What a cautious starting dose strategy looks like
- How to follow up if symptoms change or worsen
- What the renewal process looks like in your state
If you are unsure how to describe your condition or why cannabis is being considered, reviewing common qualifying reasons ahead of time can help. Our guide on good excuses to get a medical marijuana card is a useful reference for framing that discussion clearly.
A prepared appointment leads to better answers, better guidance, and a clearer path forward.
Conclusion
Telehealth and in-person consultations both have a place in medical marijuana care. Some situations call for face-to-face exams. Others benefit from hands-on support. But when you have a choice, telemedicine consistently wins on convenience and cost without sacrificing quality. It saves time, reduces expenses, and makes follow-up care easier to maintain. And if you are going the telehealth route, Quick Med Cards stands out. We are fast, affordable, and easy to work with. Our doctors are experienced, professional, and genuinely compassionate. For most patients, that combination makes telemedicine the smarter, simpler way to get certified.
Key Takeaways
- Telehealth is usually faster and more convenient because there is no travel, waiting room, or time off work.
- In-person visits offer a traditional exam experience and can be better for complex medical cases.
- Cannabis telemedicine expands access for patients who live far from certified clinics or have mobility limitations.
- Telehealth often costs less overall once travel time, missed work, and extra expenses are considered.
- Both telehealth and in-person visits must meet the same medical standard of care when done properly.
- State rules matter, and some programs limit telehealth to renewals or specific situations.
Frequently Asked Questions
Below are answers to common questions on telehealth versus in-person consultations for medical marijuana evaluations.
Is a telehealth medical marijuana consultation as valid as an in-person visit?
Yes. A telehealth medical marijuana consultation can be just as valid as an in-person visit.
That validity depends on two things. Your state must allow telehealth for your situation, and the clinician must follow the required standards. This includes verifying your identity, conducting a documented medical evaluation, and providing appropriate follow-up care. Because state rules vary, it is always smart to confirm your state’s current process before booking an appointment.
Can a doctor “prescribe” medical marijuana during a telehealth visit?
Usually no. Doctors do not issue a traditional prescription for medical marijuana during a telehealth visit.
In most state medical cannabis programs, clinicians provide a recommendation or certification instead of a prescription filled at a standard pharmacy. What happens next depends on your state and may include registry steps, card issuance, or renewal requirements. Texas is a notable exception, where qualifying patients receive an actual prescription.
Why do some states require an in-person visit first?
Because some states want a face-to-face exam to come first.
These states require an initial in-person visit to formally establish the patient-provider relationship and complete parts of a physical exam that cannot be done remotely. Kentucky is a clear example. Patients must be seen in person for their first certification, after which telehealth may be allowed for renewals or follow-ups.
What are the biggest red flags when booking an online medical marijuana evaluation?
Instant approval with little or no real medical evaluation is the biggest red flag.
Be cautious if a provider promises approval without a proper visit, relies only on an online questionnaire, skips identity or location verification, or avoids discussing risks, side effects, and follow-up care. State guidance, for example, Hawaii’s telehealth certification rules, makes it clear that questionnaires alone do not meet the medical standard of care for cannabis certification.
How can I find a reputable medical marijuana doctor near me?
Start with providers who clearly list the states they serve and follow the rules for your location.
Reputable services are transparent about where their doctors are authorized and how the evaluation works. Many also help match patients with clinicians who are legally allowed to recommend cannabis in their state. Quick Med Cards does exactly that. We connect you with expert, caring medical marijuana doctors near you who are state-certified to evaluate and recommend cannabis treatment when appropriate.
The process follows a clear, step-by-step flow:
- Complete a short questionnaire with your basic information.
- Create your account to access scheduling and records.
- Choose a convenient appointment time that fits your schedule.
- Meet with a qualified cannabis doctor who can assess your eligibility properly.
This structured process keeps the evaluation simple, compliant, and focused on real medical care.
Disclaimer: This article is for informational purposes only and is not medical or legal advice. Medical marijuana rules vary by state and may change. Always consult a licensed clinician and confirm your state program requirements before starting or changing any treatment.
Get Your Medical Marijuana Card
Same-day appointments available for online medical marijuana evaluation.
Get your certification now!
